Today, gynaecologists are increasingly focused on improving women’s quality of life and preserving sexual function. Minor problems can be treated with injections or laser procedures, but laparoscopy – minimally invasive surgery – still plays an important role in managing larger conditions. One such condition is uterine prolapse, or pelvic organ prolapse, for which effective treatments are available with good outcomes.
The pelvic floor is made up of a collection of muscles and ligaments that hold adjacent organs in position. The pelvic floor is often compared to the surface of a trampoline, which can lose its elasticity and become loose due to gravity, pressure build-up in the abdomen, and other factors. If these muscles and ligaments loosen too much, the organs slip down the path of least resistance – the vagina.
It is not known exactly how common this condition is. Some studies show that up to 40% of women have vaginal prolapse after removal of the uterus. It is estimated that around one in ten women will have surgery for a pelvic organ prolapse in their lifetime.
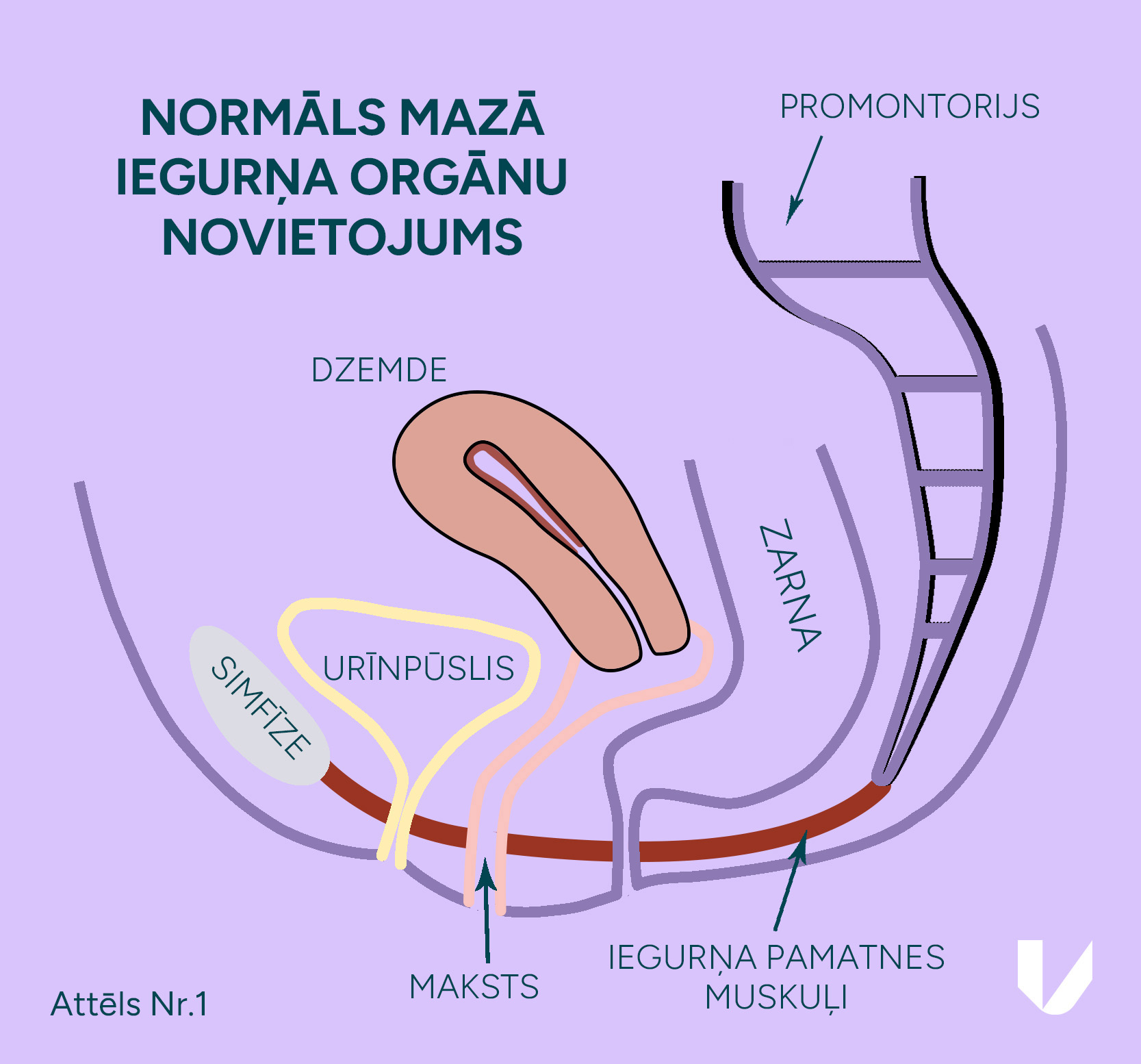
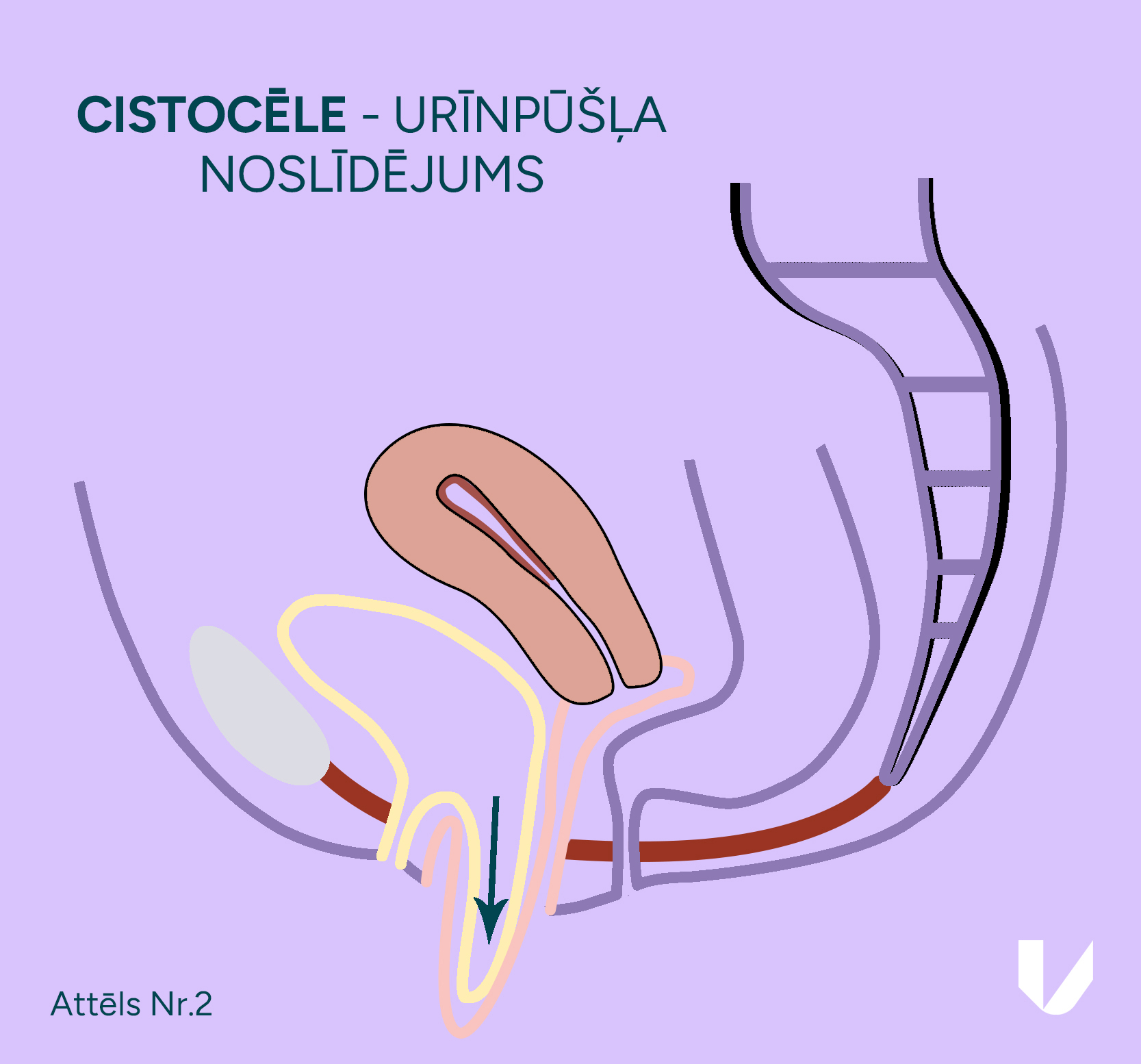
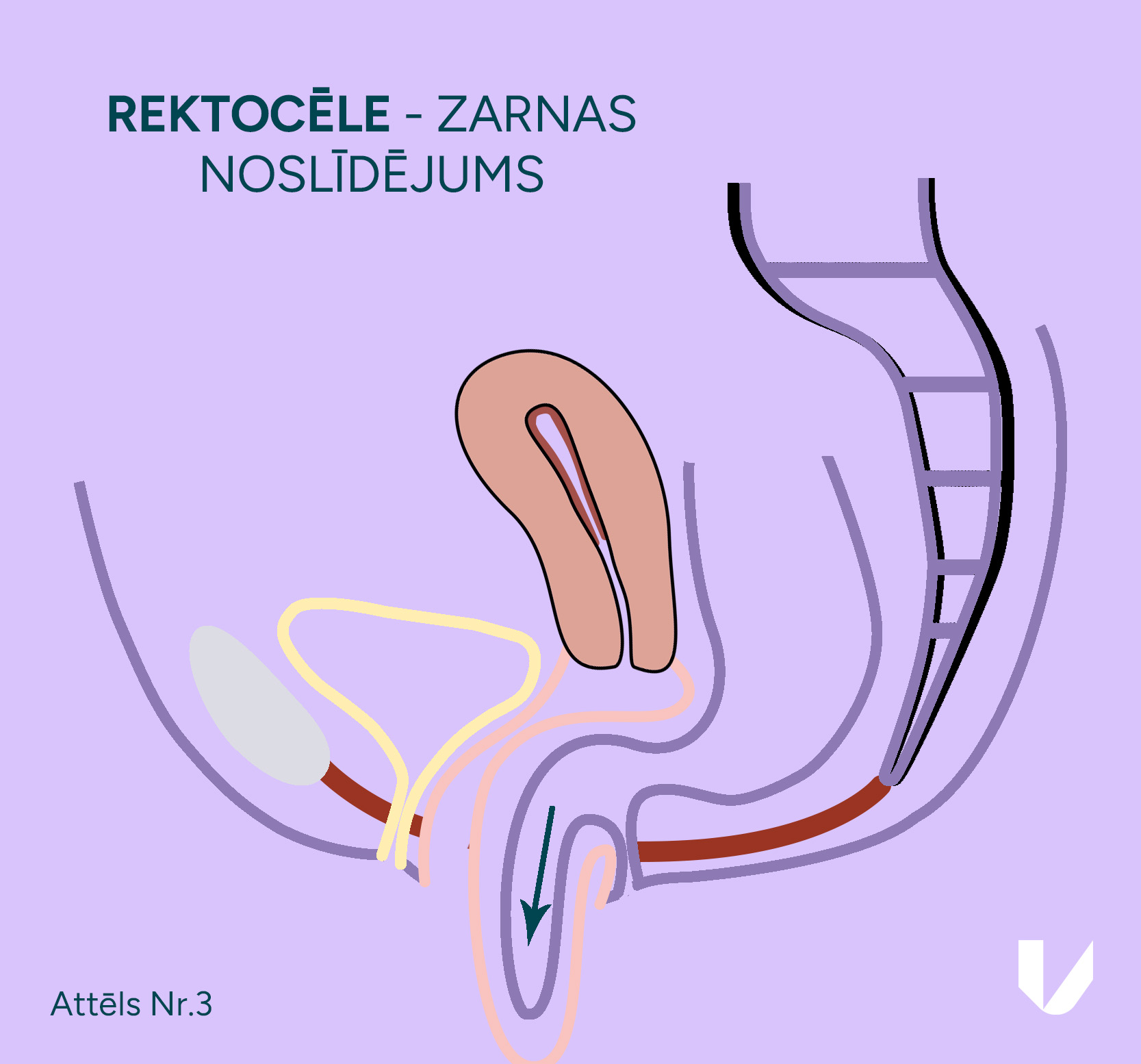
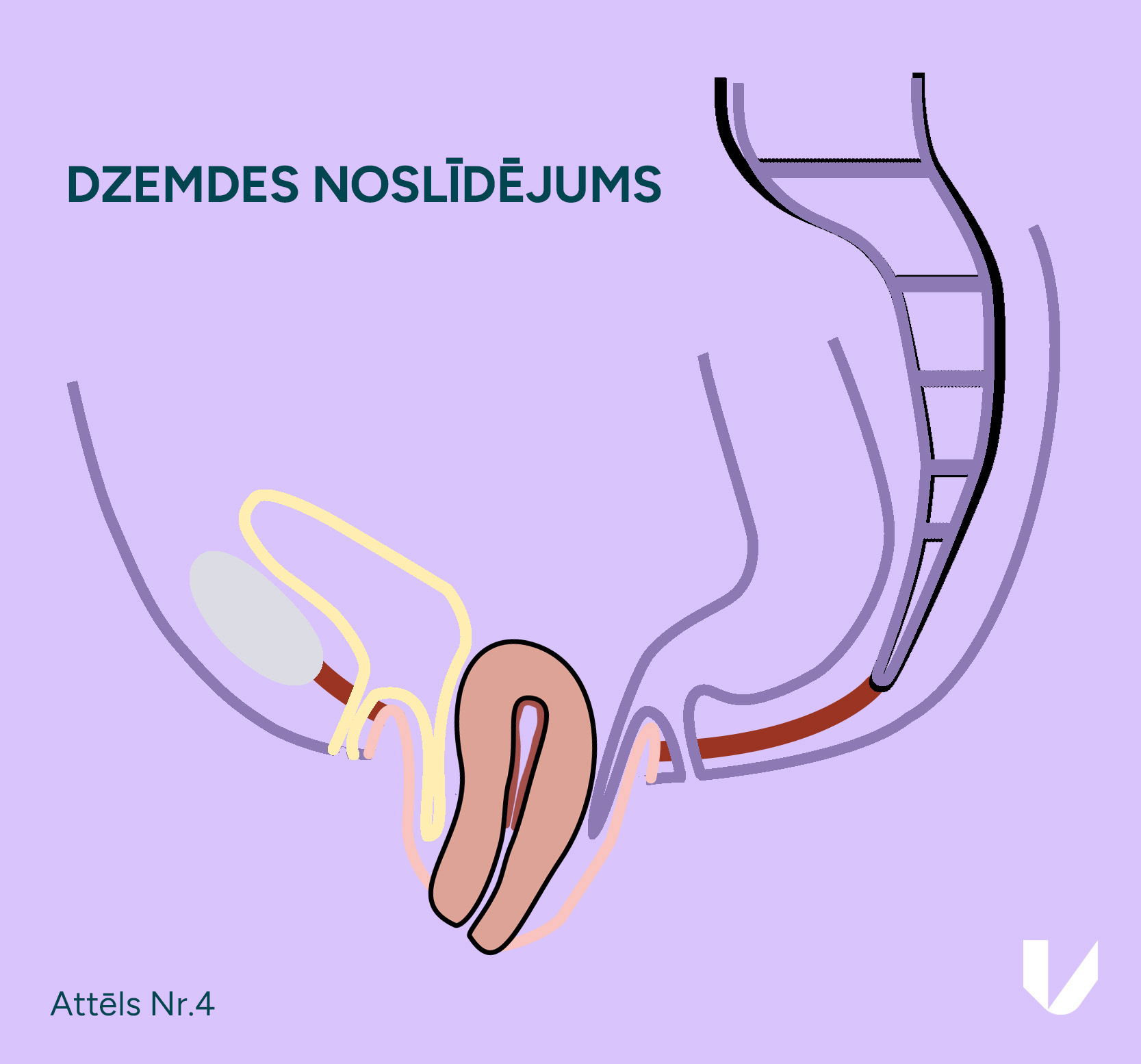
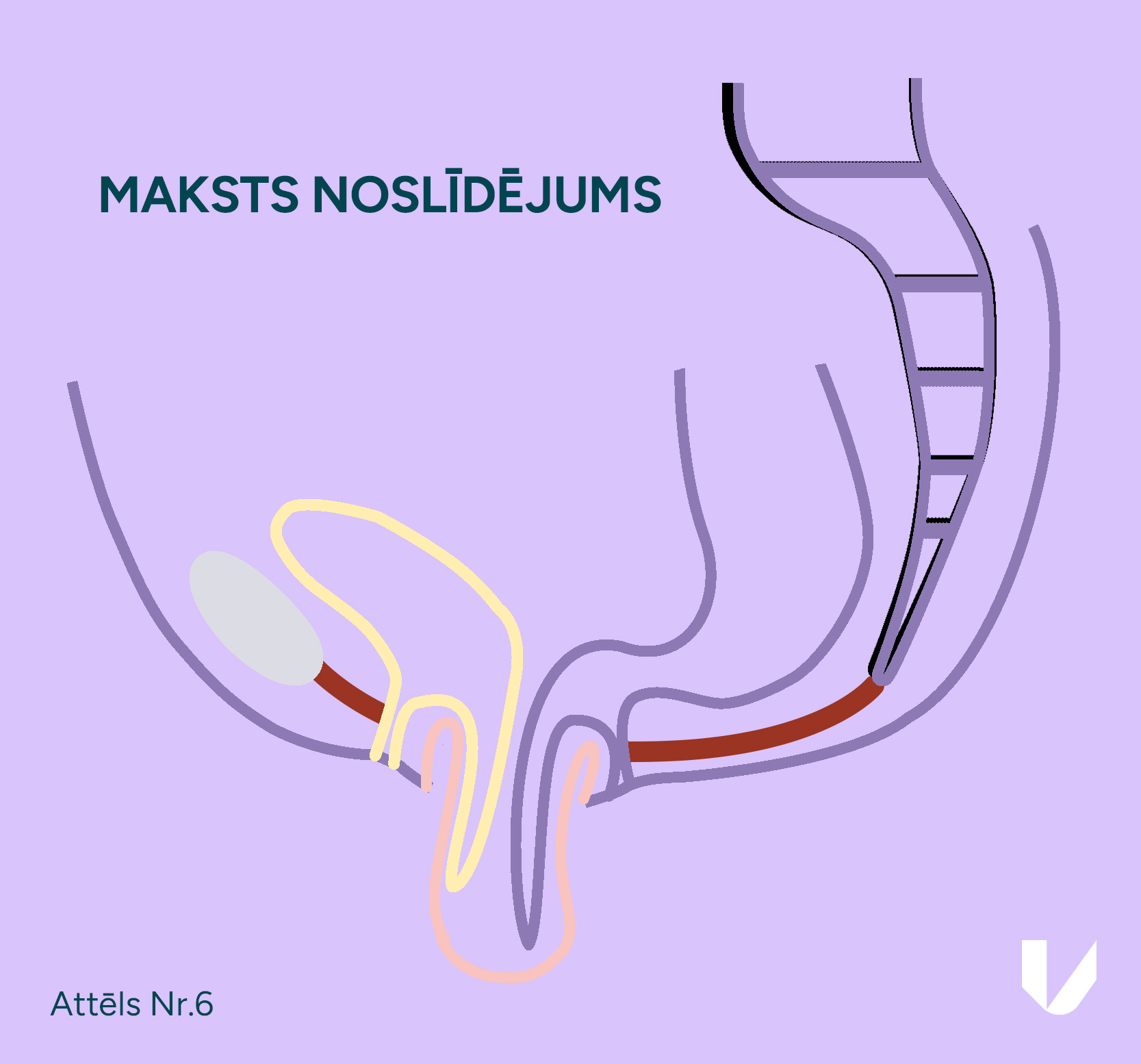
Depending on the type of prolapse, or which organ is prolapsing, they are given different names. If the bladder squeezes through the vagina, it is called a cystocele. If the rectum falls out – a rectocele. Prolapse of the uterus means that the body of the uterus and cervix fall out. In cases where there has been previous surgery to remove the uterus, the vagina may fall out, or just the cervix if it is retained during surgery. Very often, different types of prolapse are combined; for example, the bladder and the uterus can prolapse together.
The severity of the prolapse is measured in grades. Grades I and II are when the prolapse is still within the vagina. In such cases, the symptoms of prolapse may also appear. In the case of grade III and IV prolapse, the vaginal wall is externally dislocated, for example, during severe coughing or abdominal distension.
Pelvic organ prolapse is more common in menopausal women and in those with congenital connective tissue disorders characterised by ligament weakness. Risk factors also include pregnancy and childbirth. In particular, the risk of prolapse may be increased by the delivery of a large foetus, as well as by instrumental assistance during labour (vacuum extraction or forceps delivery), which can damage the pelvic floor. However, it should be noted that pelvic organ prolapse is also possible in women who have not given birth.
Greater attention should be paid to risk factors that are within a woman’s control, known as modifiable risk factors. These include smoking, obesity, extreme thinness and frequent constipation. A balanced diet is important – make sure to include plenty of fibre and plenty of fluids. Prolapse is more common in women who do weightlifting and when steroidal anti-inflammatory drugs are taken regularly. Chronic lung disease with frequent coughing can also contribute to prolapse, so the adequate treatment of such conditions is important. The risk is increased in women after a laparoscopic or abdominal hysterectomy (removal of the uterus) with or without the removal of the cervix. In such cases, it is important to suture the vaginal dome or cervix correctly to reduce the risk of prolapse.
The symptoms of pelvic organ prolapse are the main determinant of the treatment method required. This may present as a feeling of pelvic pressure, sometimes accompanied by pain. Patients often feel or can touch a mass protruding from the vagina, which may become abraded over time. If urine leakage is present when coughing or laughing, or if there is a sudden need to urinate or you have to push the mass back into your vagina to pass urine, a prolapse may be to blame. With bowel distension, difficulty passing stool may occur. In general, the greater the prolapse, the more pronounced the symptoms, and they tend to worsen over time. When you go to the doctor, it is important to describe your symptoms accurately so that the specialist can offer you the most appropriate treatment.
To prevent the risk of or reduce minor prolapse, the muscles that keep the organs in the correct position can be exercised using Kegel exercises.
They are based on the repetitive tensing and relaxation of muscles. To understand which muscles to tense, imagine you are sitting on a ball and try to lift it off the chair by tensing your muscles. These exercises can be done in any position – sitting, standing up or lying down. The aim of the exercise is to hold the muscle tension for about 10 seconds and repeat it 8–10 times in one go. The exercise should be performed 3 times a day, at least 4 times a week. Follow this regimen for at least 16 weeks. To maintain the effect, the exercise must be performed over a longer period of time, like any muscle workout. With time, you can try to hold the muscle tension for longer. If you are not sure how to do these exercises properly, you can seek advice from a physical therapist.
The type and degree of prolapse are assessed by the doctor during a gynaecological examination, with special consideration of your symptoms, which is often sufficient to plan treatment. During the examination, your doctor may ask you to tense your abdomen and cough in order to assess the extent of the prolapse and determine the most appropriate treatment. Depending on the patient’s age and symptoms, oncocytological examination, ultrasound, and uterine aspirate biopsy may be performed. If your symptoms are related to bowel movements, your doctor may order a defecography to assess bowel function and rule out possible proctological disease.
Non-surgical and surgical methods are available for treating prolapse. The main aim of any treatment is to reduce symptoms and improve quality of life, while preserving the normal function of the surrounding organs. If you are sexually active, it is important to restore or maintain your sexual function without impairing it. Depending on your symptoms and the degree of prolapse, your doctor will assess and suggest the most appropriate treatment method.
It is important to remember that no treatment method can guarantee 100% positive results, and recurrent prolapse is possible, but some methods have proven to be better than others.
Non-surgical treatment is offered as a first choice. For minor prolapse, Kegel exercises can be performed, but it should be understood that this is a time-consuming process, and the desired result will not be achieved for a few months. Next, the doctor may offer a pessary – a round silicone device inserted into the vagina. Depending on the symptoms, a pessary of the desired size and shape is chosen and inserted into the vagina in a compressed form, where it takes the required position and holds the organ (uterus or bladder) in the correct place. Pessaries are better for anterior wall and uterine prolapse, but less so for rectocele. It is important to clean and care for the pessary regularly, and follow-up visits with your doctor are necessary to assess the health of the vaginal walls and check for any signs of pressure ulcers.
Depending on the type of prolapse, your age and your preferences, the surgical approaches may vary. Nowadays, there are basically two options – laparoscopic and vaginal surgery. Both are offered at Vītola klīnika.
Laparoscopic sacrocolpopexy, also known as laparoscopic cervicopexy or laparoscopic sacral colpopexy, is considered the gold standard in the treatment of pelvic organ prolapse. This method is widely used throughout Europe and the USA. Dr Juris Vītols has been performing this surgery for more than 15 years. Over time, laparoscopic prolapse repair has been refined, and doctors at Vītola klīnika now perform it using the technique developed by their French colleagues, which provides better outcomes compared to other methods. For laparoscopic correction, four small incisions are sufficient. A custom-made mesh, which is finer and designed specifically for the treatment of pelvic prolapses, helps to achieve good results. However, the key to a good result is the experience of the operating gynaecologist, their knowledge of anatomy, and their laparoscopic suturing skills. The main advantages of laparoscopy are better visualisation of anatomical structures, less postoperative pain, faster recovery, and a lower risk of complications.

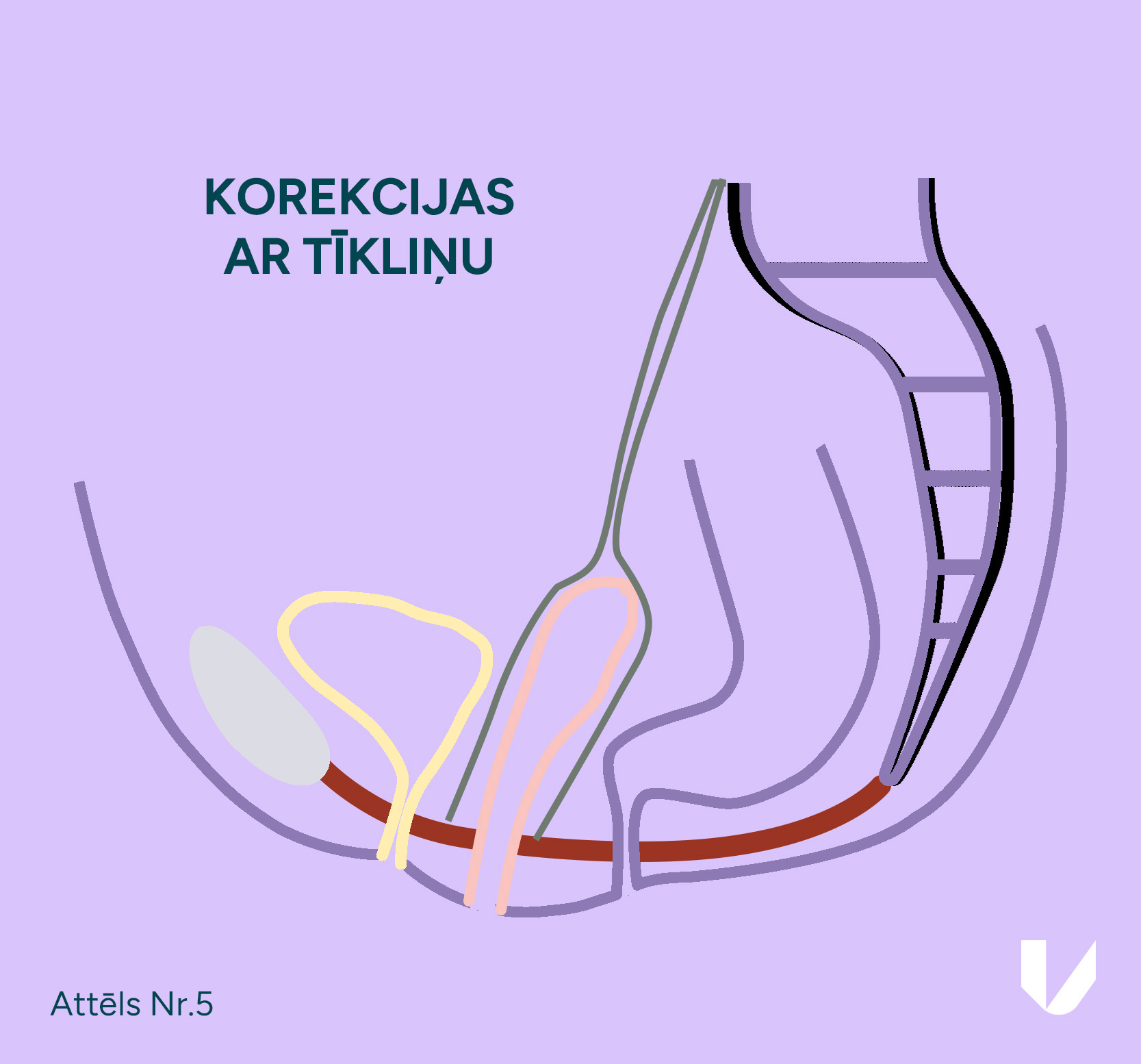
This is still a widely used approach for pelvic organ prolapse. It can treat both cystocele and rectocele, and is often used for total uterine prolapse, when the vaginal removal of the uterus and suturing of the vaginal walls is performed. Vaginal surgery can also involve the use of mesh, but we do not recommend its placement through the vaginal route because of the high risk of inflammation. In addition, these meshes are placed blindly by touch alone, unlike in laparoscopy, where direct visualisation is one of the main advantages of the technique.
However, the vaginal approach remains the primary surgical treatment for women who are not sexually active and for those with contraindications to laparoscopic surgery.
Pelvic organ prolapse is a common condition that can significantly reduce quality of life and may also lead to the functional impairment of nearby organs if not corrected in time.
To reduce the risk of prolapse, we recommend that women of all ages address potential risk factors early and perform Kegel exercises to strengthen the pelvic floor. Unfortunately, pelvic organ prolapse cannot be predicted. Sometimes, even after one completely normal and non-traumatic birth, the uterus can completely prolapse. It is important to remember that this is not a normal situation, and in such cases, you need to consult an operating gynaecologist. The good news is that there is a solution to this problem for women who want to maintain the possibility of carrying a child. We believe that laparoscopic sacrocolpopexy is the most effective treatment, but each woman’s symptoms and needs should be assessed individually. A pessary or simple anterior vaginal wall surgery may be sufficient to help you maintain a full and high-quality life.
The gynaecology and surgery clinic Vītola klīnika is built on the extensive experience of Dr Juris Vītols and the excellent teamwork that forms an essential part of comprehensive patient care. Since performing the first gynaecological laparoscopic surgery in 1994, Dr Juris Vītols has carried out more than 10,000 endoscopic procedures. In 1995, Dr Juris Vītols was the first in Latvia to perform a laparoscopic hysterectomy. Dr Juris Vītols is also a pioneer in the laparoscopic treatment of endometriosis. Thanks to close cooperation with surgeon Dr Kaspars Snipe, Vītola klīnika has the most extensive experience in Latvia in the laparoscopic treatment of deep endometriosis, including cases requiring bowel resection.
For 5 years, the son of Dr Juris Vītols – Jurģis Vītols – has been involved in the work of the clinic. He also specialises in gynaecological surgery, particularly laparoscopy and hysteroscopy, having gained additional expertise during his fellowship in France and through regular participation in gynaecological endoscopy congresses and seminars across Europe.
Vītola klīnika offers the widest range of laparoscopic gynaecological surgeries in Latvia. We offer surgical treatment for endometriosis, including cases requiring the extensive excision of deep lesions, which are often the cause of severe pain. We also offer the laparoscopic correction of uterine prolapse, myomectomy (removal of fibroid nodules of various sizes while preserving the uterus), removal of ovarian cysts, restoration of tubal patency, adhesiolysis (removal of adhesions), correction of urinary incontinence, vaginoplasty for women with congenital absence of the vagina, correction of caesarean section scar defects (niche), as well as other complex laparoscopic operations. Surgical treatment for postpartum perineal injuries is also available.
CALL US:
+371 26 412 412Consultation with an experienced doctor is the first step towards taking care of your health and well-being.
AIZPILDIET PIETEIKUMA FORMU: