Uterine fibroids (also called fibroids or nodules) are the most common benign uterine tumours. Treatment is indicated when fibroids cause symptoms, and treatment decisions must be made especially carefully in women planning pregnancy. The main modern treatment in such cases is myomectomy – the laparoscopic or hysteroscopic removal of the fibroid. If pregnancy is no longer planned, several treatment options are available, including fibroid embolisation, medical therapy, or hysterectomy (removal of the uterus). In this article, we will look at laparoscopic and hysteroscopic myomectomy, which is a uterus-preserving surgery that Dr Juris Vītols has been performing since 1998. Dr. Juris Vītols veic jau kopš 1998. gada.
There is a misconception that small fibroid nodules, which do not deform the uterine cavity, have no impact on fertility. Studies have shown that even fibroids as small as 3 cm, which do not deform the uterine cavity, can contribute to infertility and recurrent miscarriage. Even in the absence of pain or bleeding, a fibroid may cause inflammatory changes in the uterine wall, potentially affecting both conception and the continuation of pregnancy.
It is important to note that the risks associated with pregnancy vary depending on the size and location of the fibroid:
More important than the size of the fibroid is its position within the uterine wall, as this determines both the symptoms and the appropriate surgical approach – laparoscopy or hysteroscopy. The FIGO (International Federation of Gynecology and Obstetrics) classification (see next figure) is used to describe the localisation of uterine fibroids and divides fibroids into 8 types and one hybrid type (2–5). Gynaecological ultrasound is an excellent tool for determining the size and location of uterine fibroids. In more complicated cases, an MRI may be needed.
In the case of type 0, 1 and 2 fibroids (sometimes also type 3), hysteroscopic resection of the fibroid is necessary. Other types require the laparoscopic removal of the fibroids, including in the case of a hybrid fibroid, which is sometimes mistakenly assessed as hysteroscopically treatable.
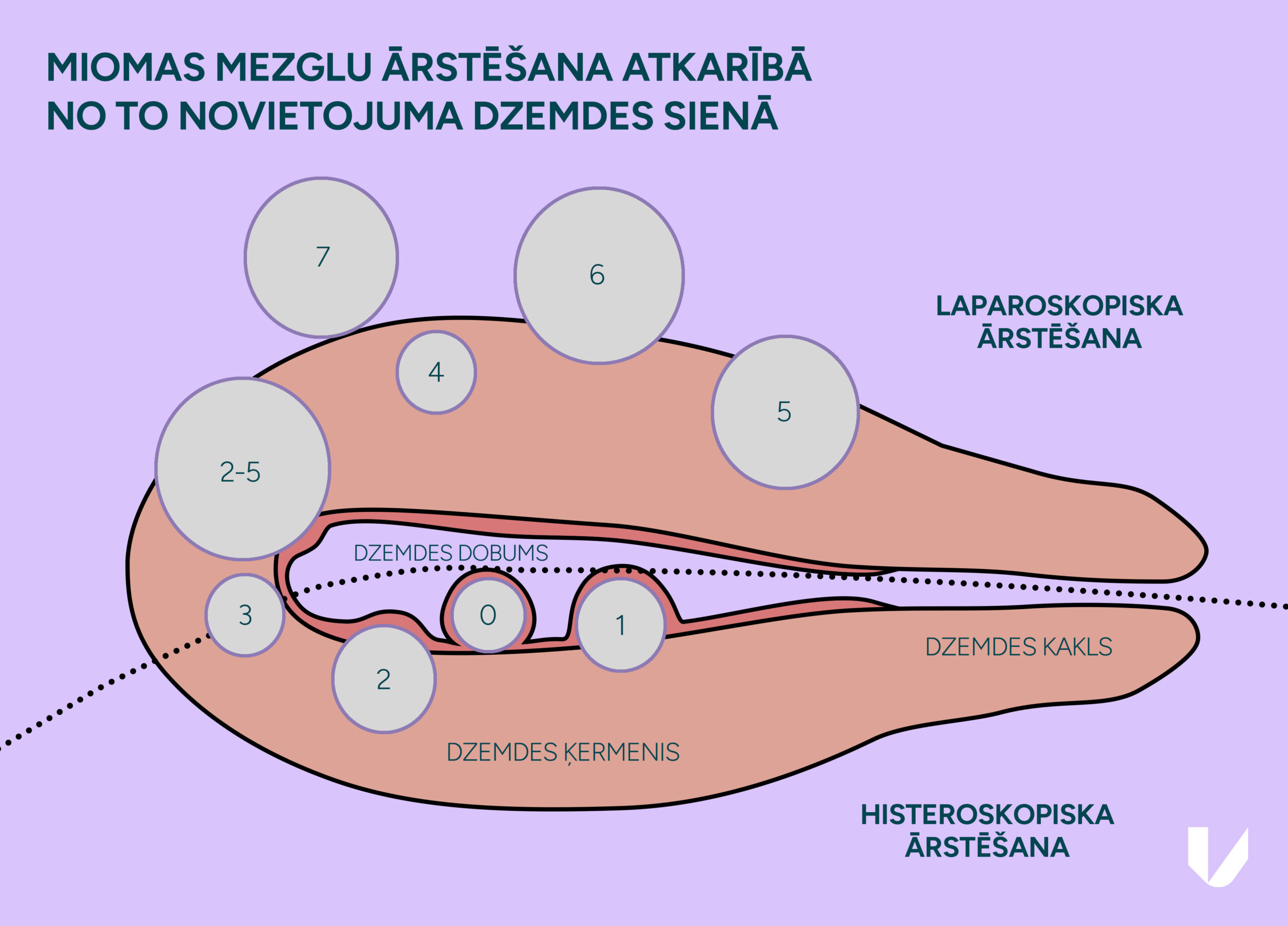
When different types of fibroids are present in the uterus, both laparoscopic and hysteroscopic myomectomy can be performed during the same operation.
This treatment method is the gold standard for types 3 to 8 and hybrid fibroids. Laparoscopic myomectomy is performed under general anaesthesia through three to four small (0.5–1 cm long) incisions in the lower abdomen. Surgery involves several steps, the most important being the removal of the fibroid and suturing of the myoma bed. Identifying the correct surgical plane during fibroid removal is crucial to ensure proper healing, minimise bleeding, and reduce the risk of recurrence. The most important step of this operation is suturing the site of the removed fibroid, which can be performed laparoscopically with excellent outcomes. The quality of the suturing is determined by the skills and experience of the chosen laparoscopic specialist. Dr Jurģis Vītols has also proven his skills at the European level, when in 2018, he won the ESGE (European Society for Gynaecological Endoscopy) Winners Programme in the laparoscopic suturing competition. After the surgery, the patient can eat and move freely in the evening and go home the next day.
Like any other laparoscopic surgery, laparoscopic myomectomy has various advantages over laparotomy (open surgery with incision). Laparoscopic surgery has:
It is a misconception that fibroids larger than 6–7 cm cannot be removed laparoscopically. The specialists at Vītola klīnika also successfully treat fibroids larger than 10 cm. If necessary, various techniques can be used during laparoscopy to minimise bleeding, such as the temporary clipping of blood vessels.
However, laparoscopic myomectomy also has its limitations and may not be feasible in cases where:
However, each case must be assessed on its own merits, as the location of the fibroid is more important than its size. Fibroids larger than 12 cm can also be removed laparoscopically if they are located in an easily accessible location.
One of the postoperative risks of laparoscopic myomectomy is the possibility of uterine rupture during pregnancy. However, according to various studies, it is less common than in women who have had a previous caesarean section, and is less than 0.5%. The main risk-mitigating factors are the use of little coagulation and the adequate suturing of any fibroid bed.
Pregnancy planning recommendations are offered on a case-by-case basis. Depending on the size and number of fibroids, we recommend that patients avoid getting pregnant for at least 3–6 months after surgery. The way the baby will be delivered must be decided after the surgery. It is a misconception that vaginal delivery is contraindicated after fibroid removal involving entry into the uterine cavity, as this does not significantly increase the risk of rupture. As several studies have shown, there is no correlation between the opening of the uterine cavity and the risk of rupture. The key factor is the proper suturing of the fibroid bed and minimal coagulation. After the removal of very large and multiple fibroids, we recommend that the pregnancy is resolved by elective caesarean section.
In the case of large and fast-growing fibroids, there is a risk of malignancy. Currently, there is no conclusive method to accurately predict the nature of the fibroid before surgery. For young women, the risk is minimal. Caution should be exercised in premenopausal and postmenopausal women with a rapidly growing fibroid. In such cases, myomectomy is not recommended, and a hysterectomy should be performed.
Hysteroscopic fibroid resection (excision) is performed for type 0, 1 and 2 fibroids (sometimes also for type 3), and is necessary for fibroids that are already small in size. They often cause symptoms, most commonly, heavy menstrual bleeding or a failure to become pregnant.
The surgery is performed under temporary anaesthesia, when a special instrument is inserted through the cervix into the cervical cavity and used to cut out the fibroid under visual control. Resection of fibroids larger than 3–4 cm may require two or more procedures to remove all the tissue, as hysteroscopy is generally limited to under one hour to minimise surgical risks. After surgery, we often insert a special gel into the uterine cavity to reduce the formation of adhesions. The patient can go home in the evening of the day of surgery.
After hysteroscopic or laparoscopic myomectomy of large fibroids – particularly when the uterine cavity has been opened laparoscopically – we recommend a diagnostic hysteroscopy within 4–6 weeks to identify and remove any adhesions. They can be divided immediately, helping to preserve fertility and support a successful future pregnancy.
At Vītola klīnika, our specialists offer unmatched experience in Latvia in the laparoscopic and hysteroscopic removal of uterine fibroids. This type of treatment ensures a better post-operative period and reduces the risks of surgery. For a more effective and successful outcome, we encourage early diagnosis and, if necessary, treatment.
CALL US:
+371 26 412 412Consultation with an experienced doctor is the first step towards taking care of your health and well-being.
AIZPILDIET PIETEIKUMA FORMU: