Uterine removal, or hysterectomy, is one of the most common gynaecological operations performed for both benign and malignant conditions. Nowadays, especially for benign diseases, a minimally invasive surgical approach – laparoscopy – is preferred.
The most common benign conditions requiring hysterectomy are uterine fibroids and adenomyosis (endometriosis of the uterine wall), particularly when they cause heavy bleeding, severe pain, or rapid uterine enlargement. When a hysterectomy is performed for a benign disease, the cervix and, depending on the woman’s age, the ovaries can often be preserved. Currently, to help reduce the risk of ovarian cancer, the fallopian tubes are often removed at the time of hysterectomy. After this surgery, menstrual periods will stop. However, if the cervix is preserved, some women may occasionally experience light, cyclical bleeding. After a hysterectomy, it is no longer possible to become pregnant, and contraception is not required.
Laparoscopy is a minimally invasive surgical technique that offers several benefits, not only for small but also for large uteri. The most noticeable benefit is reduced post-operative pain, which allows most patients to go home the day after surgery and return to their normal activities much sooner.
For various uterine symptoms, removal of the uterus is the most effective treatment. Studies show that even among women who were uncertain beforehand, about 95% are satisfied with their decision to undergo a hysterectomy.
This surgery is performed under general anaesthesia. During the procedure, 3–4 small incisions (each up to 1 cm) are made in the abdominal wall. Through these, the surgeon performs the operation using a camera and specialised laparoscopic instruments. Depending on the type of hysterectomy and the size of the uterus, it may be removed either through the vagina or through small incisions in the abdomen using a special device that divides the uterus into smaller pieces. To safely perform a laparoscopic hysterectomy, the surgeon’s skill in laparoscopic suturing is important. Proper closure of the vagina or cervix helps reduce the risk of vaginal prolapse. Laparoscopic removal of the uterus is the ‘gold standard’ in modern gynaecological surgery. Even a large uterus is not necessarily a barrier to performing the procedure with this method. At Vītola klīnika, this method is used in 99% of cases. In addition to a laparoscopic hysterectomy, the surgeon can also correct vaginal wall prolapse and treat urinary incontinence using minimally invasive techniques.
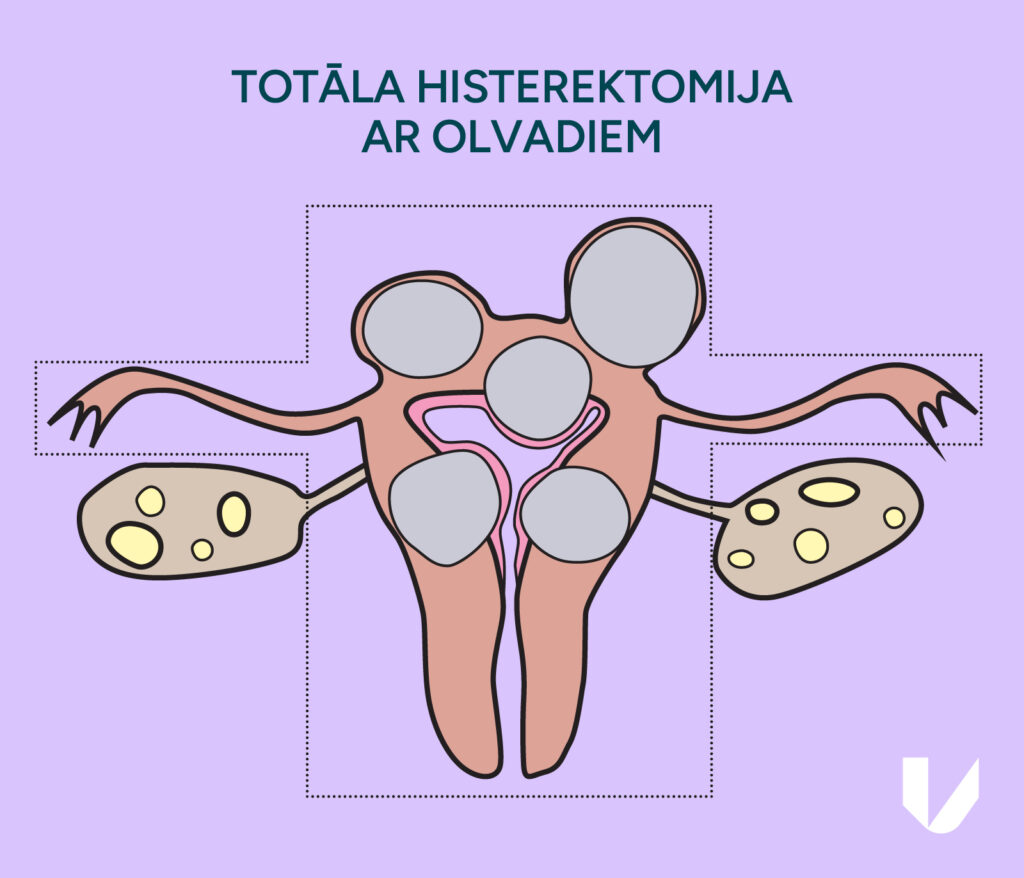
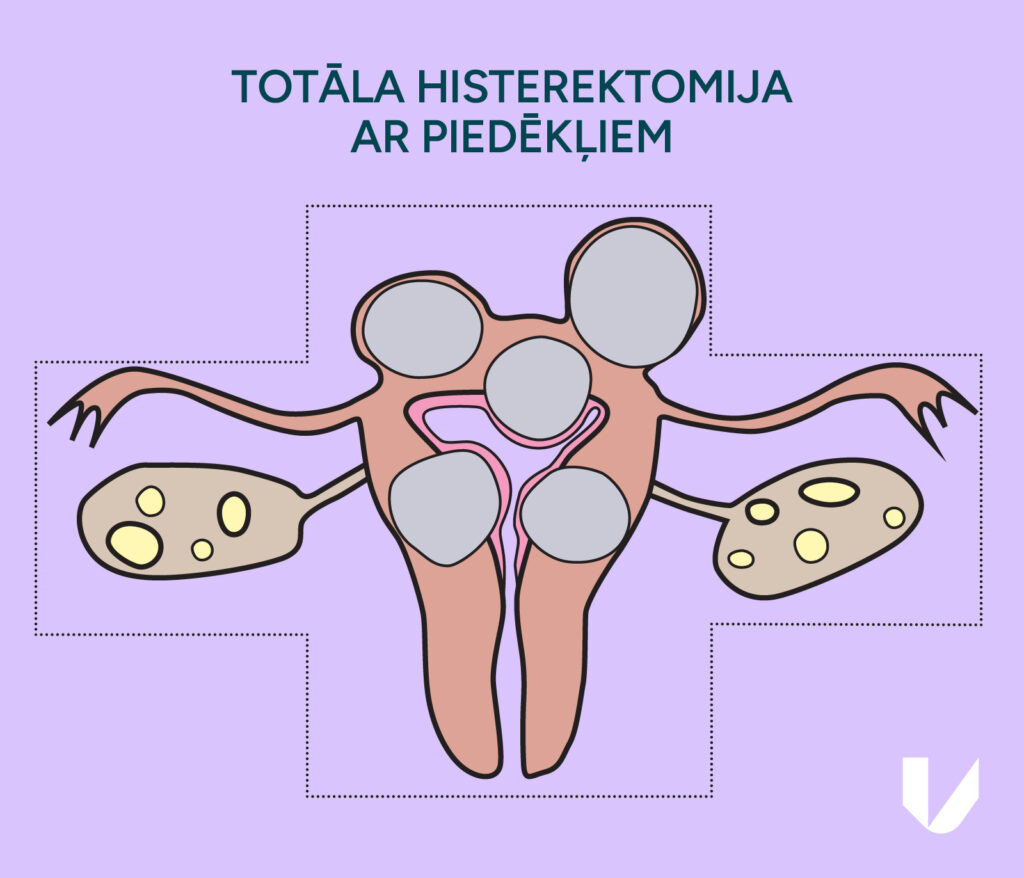
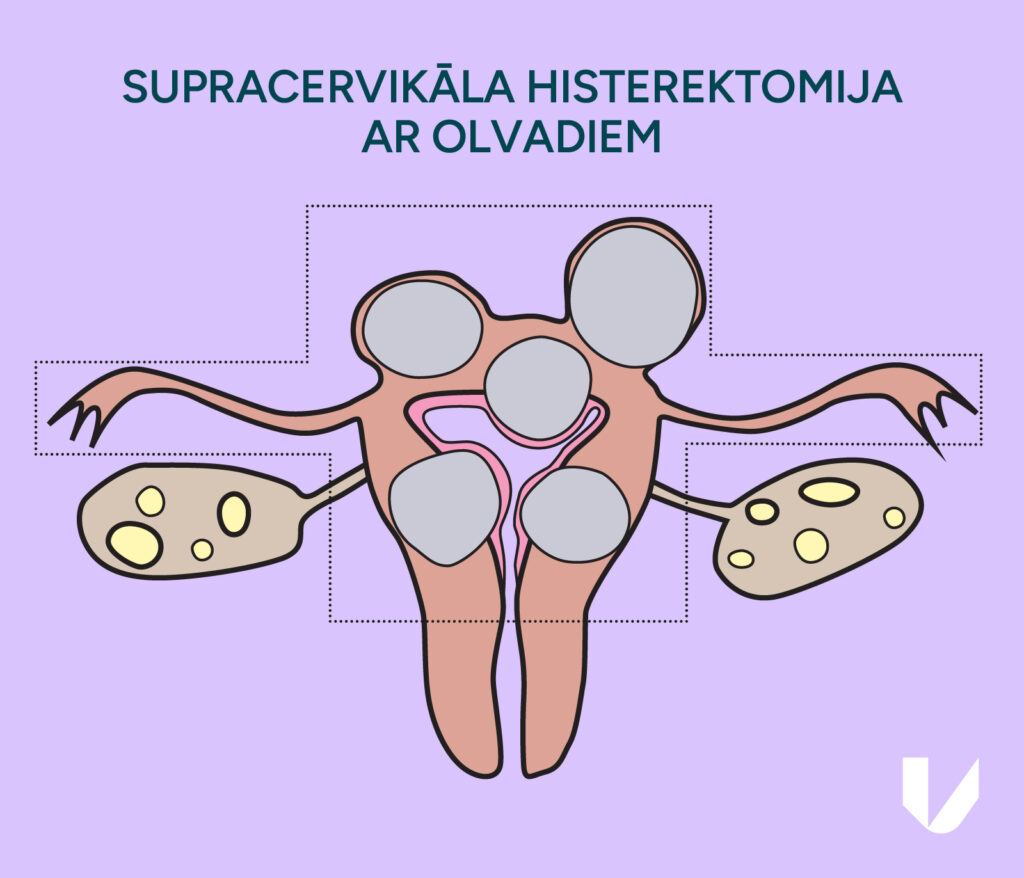
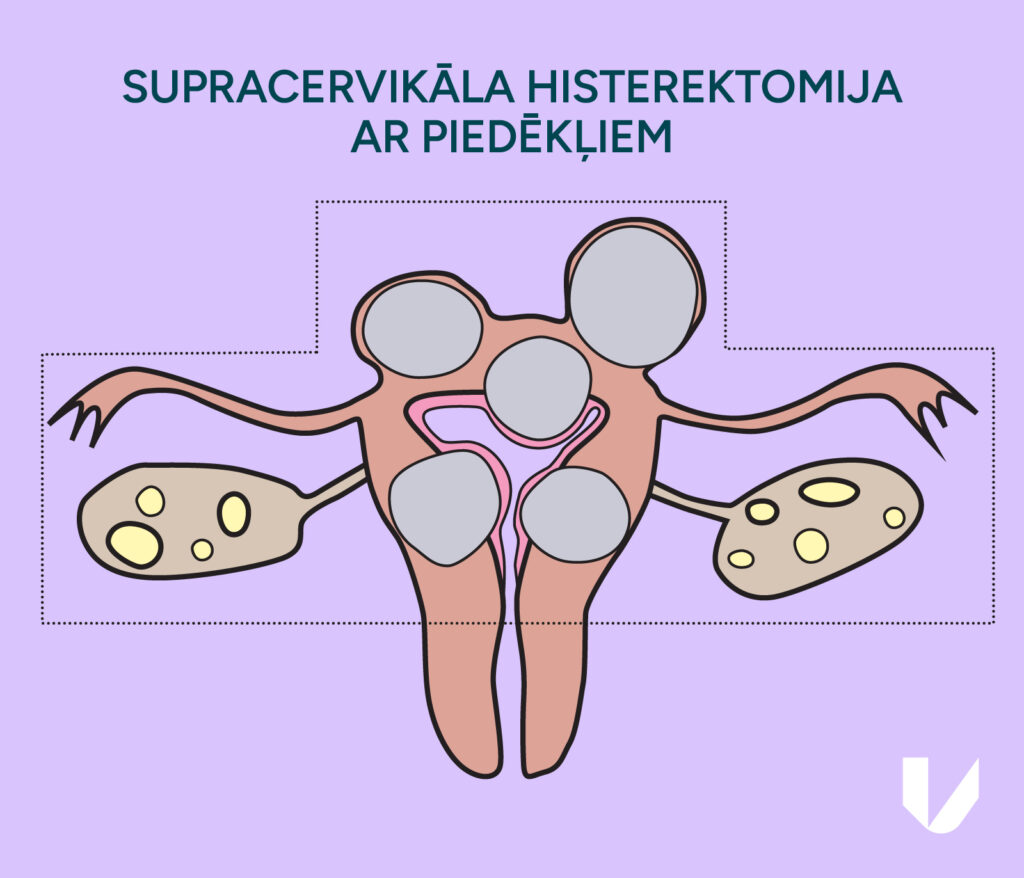
Research shows that there is little difference in outcomes between a total hysterectomy and a supracervical hysterectomy. For example, there is no evidence of differences in quality of life, as well as differences in sexual life, such as achieving an orgasm.
In cases where the cervix is retained, cyclic bloody discharge may sometimes continue. Cervical cytology should also be continued after surgery as a screening test for cervical cancer.
One of the most widely used procedures today is laparoscopic surgery to treat uterine or vaginal prolapse, as well as urinary incontinence.
You can read about the treatment of uterine prolapse in another article.
Stress urinary incontinence (stress incontinence) is the most common type of urinary incontinence in women. Its incidence increases with age, and some literature suggests that 1 in 3 women will develop urinary incontinence in their lifetime. Stress urinary incontinence is the involuntary leakage of urine that occurs during physical activities such as coughing, laughing, exercising, or lifting. It is caused by changes in the normal position of pelvic organs and weakening of the pelvic floor. Urinary incontinence can greatly affect quality of life and often leads women to avoid the activities they enjoy. Depending on how severe the incontinence is, it can be treated with pelvic floor exercises or surgery. At Vītola klīnika, we offer laparoscopic Burch surgery for the treatment of stress urinary incontinence. During the procedure, the angle between the bladder and urethra is restored with special stitches, helping to prevent urine leakage. This is a well-established technique that is becoming popular again, especially since vaginal mesh surgery has been banned in the United Kingdom and the United States due to the high risk of complications. The effectiveness of the surgery is ~85–90%, and the risk of complications is much lower with an experienced surgeon.
The laparoscopic approach ensures the patient’s full recovery in a much shorter period of time. Much less pain relief is needed after such surgery compared to incisional surgery. After the laparoscopic removal of the uterus, most patients can return home the next day to recover in the comfort of their usual environment, which helps speed up healing. Pain relief therapy is provided in the clinic immediately after surgery. The patient can slowly get to her feet a few hours after waking up from surgery. Depending on her needs, the patient may continue taking over-the-counter pain relievers for the first 3–5 days after returning home. During the first two weeks after surgery, patients gradually regain their energy by slowly increasing activity levels while making sure to rest adequately. During this time, it is very important to consume enough fluids. Most patients are able to carry out full activities and resume sexual activity after about 6 weeks. Before fully returning to your normal routine, it’s best to consult your doctor, since recovery varies from person to person and depends on several factors.
CALL US:
+371 26 412 412Consultation with an experienced doctor is the first step towards taking care of your health and well-being.
AIZPILDIET PIETEIKUMA FORMU: