Endometriosis is a condition in which tissue similar to the uterine lining (endometrium) grows outside the uterus, leading to chronic inflammation.
Pain is the most common symptom of endometriosis. Most often during menstruation, sexual intercourse, and gastrulation.
Often, this pain is cyclical and depends on the day of your period. Over time, it may persist and occur independently of the menstrual cycle. Symptoms may become so severe that they interfere with daily activities and significantly affect quality of life.
Infertility is the second most common concern among women of reproductive age. It is estimated that 30–40% of women with endometriosis will require assisted reproduction, such as in vitro fertilisation (IVF).
The prevalence of endometriosis is not precisely known. It is estimated that about 5–10% of women of reproductive age have endometriosis that causes symptoms and requires some form of treatment. If a woman experiences both severe pain (most often during menstruation) and infertility, endometriosis is diagnosed in up to 50% of cases.
There are several theories about how and why this condition occurs. None of them is fully proven, and none of them explains how endometriosis develops. Multiple interacting factors likely contribute to the development of endometriosis, rather than a single cause.
Retrograde menstruation, or the backflow of menstrual blood, is the oldest and most popular theory of the origin of endometriosis. However, this alone cannot explain the development of this disease, as nearly all women experience some menstrual blood in the abdominal cavity, yet only some develop endometriosis as a condition.
Metaplasia is the transformation of one type of normal tissue into another. This helps explain why endometriosis can sometimes appear in areas where menstrual blood doesn’t flow back to, such as the tissue between the rectum and vagina (the rectovaginal septum). Some experts suggest that these changes originate during embryonic development, while others believe certain adult cells may retain the ability to transform into different types.
As mentioned above, small fragments of endometrium may enter the abdominal cavity with retrograde menstrual flow, but not all women develop endometriosis as a result. This is supported by the immune system malfunction theory, which suggests that when the immune system is functioning normally, displaced endometrial cells are destroyed outside the uterus. In addition, the immune system is believed to be influenced by adverse environmental factors, such as processed foods, everyday chemicals, and other exposures.
Studies show that women with first-degree relatives diagnosed with endometriosis have a higher risk of developing the condition themselves. In such cases, the disease is likely to have more pronounced symptoms.
There is a theory that endometrial fragments can spread through the bloodstream or lymphatic system. This would explain how endometriosis can develop in the lungs, brain, or other organ systems.
Endometriosis can take different forms. All types of the disease can be diagnosed by laparoscopy – a minimally invasive surgical technique that allows both diagnosis and treatment. Ovarian cysts and larger lesions of deep endometriosis are clearly visible on the ultrasound. Detection of superficial and smaller typical lesions without surgery is limited. Endometriosis is often diagnosed late, as laparoscopy is usually only performed when lesions are large enough to be detected by ultrasound or MRI, and medical treatment is no longer effective.
According to one theory of endometriosis development, subtle lesions represent the initial stage of the disease and are found in up to 80% of women with the condition. They do not cause symptoms and can be discovered accidentally. Not all cases will progress to other types of endometriosis because the body’s own defence mechanisms prevent this from happening. These are small, white, pink or transparent lesions, about 1–3 mm large. If the surgeon lacks experience in treating endometriosis, lesions may be misinterpreted during laparoscopy, leading to an incorrect diagnosis. It is important to identify subtle lesions, as they can sometimes conceal deeper foci of endometriosis that should be excised due to the symptoms they cause. These subtle lesions cannot be seen by ultrasound or MRI.
Typical endometriosis lesions can be 0.5–4 cm in size and, depending on their location, can cause pain during menstruation, during intercourse, and in other cases. Such lesions may be found on the bladder, uterine ligaments, at the site of ovarian adhesion, on the diaphragm, and elsewhere. Visually, they appear brownish black with whitish fibrosis in the periphery.
The main treatment for typical endometriosis lesions is laparoscopic complete excision (coagulation or “cauterisation” is proven to be ineffective and pointless). This can be a time-consuming and complicated process, as it may require the ureters and nerves to be cleared of adhesions. Once they are completely cut out, there is very little risk of them recurring (new ones are more likely to form than old ones to return). Depending on the size and location of them, and the doctor’s experience in examining endometriosis, they can be diagnosed using gynaecological ultrasound and magnetic resonance imaging.
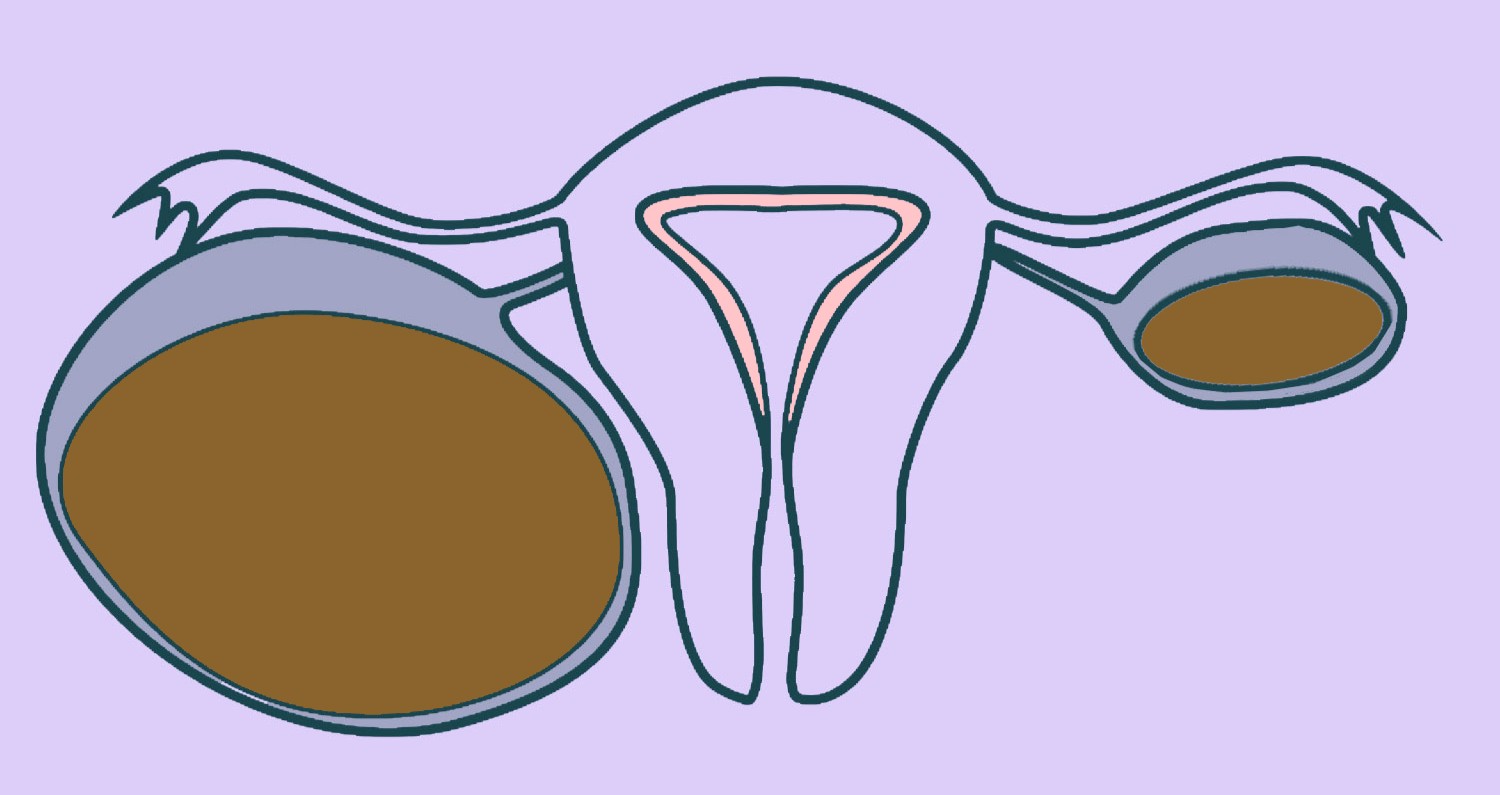
Cystic endometriosis most often forms in the ovaries and forms so-called “chocolate” cysts. They can be as large as 10 cm and can be present in both ovaries at the same time. The cysts contain a dark brown, thick, chocolate-like substance formed from old blood that accumulates inside the cyst. Depending on the size and the symptoms that the cyst causes, the treatment of choice is laparoscopic removal of the cyst. The precision and gentleness of surgery are crucial, as preserving healthy ovarian tissue is essential for future fertility. The specialists at Vītola klīnika emphasise that excising the lesions at the ovarian attachment site is essential to lower the risk of symptoms, the recurrence of endometriosis, and the need for repeat surgery. Cystic endometriosis can be diagnosed very well with both gynaecological ultrasound and MRI, and is usually recognised by all doctors who use either of these techniques.
If the cyst is smaller than 3 cm and asymptomatic, it may be monitored, with laparoscopic treatment postponed. However, experience shows it is a mistake to monitor small cysts (0.5–3 cm) for long periods or attempt to ‘treat’ them with hormonal therapy in cases of severe pain. These small cysts may be early indicators of more extensive disease, such as deep endometriosis lesions that cannot be detected by ultrasound or MRI.
Deep endometriosis is made up of lesions that can be as large as 5–6 cm. They are most often located behind the uterus, growing into the vagina, bladder and uterine ligaments, and can even involve the bowel wall. Such lesions almost always cause severe pain and may also cause problems with gastric transit and urination. Depending on their location, such lesions may be detected during a gynaecological examination with a speculum or through a bimanual examination. It is important that the doctor is experienced in examining such patients. Depending on the specialist’s experience, deep endometriosis can be diagnosed by gynaecological ultrasound and magnetic resonance imaging. The main treatment for this type of endometriosis is laparoscopic surgery, which involves the excision of all the lesions. If the bowel is involved, removal of part of the bowel may also be necessary.
Adenomyosis is endometriosis of the uterine wall. The main symptoms are heavy menstrual bleeding, pain, and infertility. Adenomyosis can present in two forms – diffuse (widespread) or nodular, with the latter often being mistaken for uterine fibroids. This condition can be diagnosed by both gynaecological ultrasound and magnetic resonance imaging. Surgical treatment is highly debated in cases where uterine preservation is desired and future pregnancy is planned. In our experience, laparoscopic surgery in such cases is challenging and should only be considered when medical treatment proves ineffective and no alternatives remain. Laparoscopy is best used for nodular adenomyosis when excision of the nodule is performed. If pregnancy is no longer planned and medical treatment is ineffective or not feasible, a laparoscopic hysterectomy is recommended.
| Type of endometriosis | Frequency | Pain | Infertility |
| Superficial endometriosis | 80% | no | no |
| Typical endometriosis | 25% | Approximately 50% | May worsen |
| Cystic endometriosis | 10% | Approximately 80%, strong | Common |
| Deep endometriosis | Approximately 3% | Up to 95%, very strong | May worsen |
Worldwide, endometriosis is often diagnosed late because symptoms may be non-specific, examinations incomplete, and menstrual pain is too often regarded as ‘normal.’ Endometriosis can mimic other non-gynaecological conditions, which may be identified through various tests but are not always visible on a gynaecological ultrasound. As a result, endometriosis is sometimes diagnosed more than 5–7 years after the first symptoms appear.
To consider the possibility of endometriosis, it is essential to evaluate the patient’s symptoms, their progression, and their characteristics.
Although clinical examination, gynaecological ultrasound, and MRI now provide detailed information for planning surgery, providing consultations to the patient and assessing the size and location of lesions, the only way to confirm endometriosis with certainty is through diagnostic laparoscopy and the histological examination of tissue samples. It should be noted that not all doctors recognise endometriosis when it does not have the typical appearance (brownish or pinkish lesions), as in retrocervical endometriosis, which mainly consists of fibrotic, dense tissue. In such cases, the diagnosis may be missed. Although diagnostic laparoscopy is often reserved for uncertain cases, when performed by an experienced gynaecologist, it also allows for the excision of smaller lesions during the same procedure.
Although international studies show that gynaecological ultrasound and MRI can be highly accurate in diagnosing endometriosis, these results come from specialised centres with extensive experience and large patient volumes – a level of expertise not comparable to most Latvian centres. In cases where all non-invasive examinations are uneventful and pathologies of other organs are excluded, we recommend diagnostic laparoscopy.
Current research shows that women with endometriosis have a reduced likelihood of conceiving spontaneously compared to women without the condition. Spontaneous pregnancy is possible, but the chances depend on the severity of the disease.
In cases of minimal or mild endometriosis, conception generally takes longer, and the likelihood of pregnancy is lower compared to women without endometriosis. However, in the case of moderate and severe endometriosis, the likelihood of pregnancy is even lower compared to minimal and mild endometriosis. Observational studies show that the more severe the endometriosis, the more difficult the path to pregnancy.
However, it is important to remember that endometriosis and infertility do not equate. Women with severe, untreated endometriosis may still conceive, making fertility outcomes complex and often emotionally challenging.
There is no clear reason why endometriosis can cause infertility. When endometriosis causes adhesions that densely surround or displace the ovaries and fallopian tubes, the passage of the egg into the tube may be impaired. However, even with normal organ placement, pregnancy may not occur. This may be explained by the chronic inflammatory environment created by endometriosis, which interferes with the maturation and fertilisation of high-quality eggs.
Hormonal therapy does not improve the likelihood of pregnancy during treatment for mild or severe endometriosis. Some studies suggest that shortly after hormonal treatment, the chances of pregnancy may improve. This can be explained by a momentary delay in the inflammatory process that could be the cause of infertility.
The aim of the surgery is to cut out all the endometriosis lesions and remove any adhesions that could interfere with pregnancy. Research confirms that effective surgery can improve fertility – increasing the chances of becoming pregnant naturally, as well as improving the results of assisted conception. It is important to have this treatment with a doctor who offers the complete excision of the endometriosis lesions.
In the case of ovarian endometriotic cysts (endometriomas), there is considerable debate regarding the optimal timing of surgery. Some studies suggest that removing cysts larger than 3–4 cm significantly improves the chances of pregnancy. Removing the cyst through careful excision or scraping achieves significantly better outcomes than simple drainage and flushing. Cyst removal also enables histological diagnosis and facilitates egg retrieval if IVF is required.
Patients should be aware that cyst removal may reduce the ovarian reserve, which is an important factor in planning future pregnancies. It is therefore essential to choose a highly experienced specialist from the outset to minimise the risk of ovarian damage and recurrence of endometriotic cysts. Often, treating a cyst also means removing the original lesion on the pelvic wall, which can be technically complex because of nearby structures like the ureter, blood vessels, and nerves.
If a cyst recurs and repeat surgery is required, the risk of ovarian damage increases significantly, which may seriously compromise future fertility. In such cases, the benefits and risks must therefore be carefully weighed. In cases of recurrence, an alternative approach is vaginal cyst puncture with a special rinse, which can be used as preparation for IVF.
As mentioned above, endometriosis patients often have difficulty getting pregnant. Surgery and medical treatment do not always lead to spontaneous pregnancy, but in such cases, they significantly improve the outcomes of in vitro fertilisation (IVF).
The aim of endometriosis treatment is to relieve pain and restore the function of the organs involved. If the patient wishes to become pregnant, surgery can improve the chances of pregnancy.
There are two methods of treating endometriosis – medical and surgical.
When no significant damage to surrounding organs or large ovarian cysts is present, or when the patient does not wish to undergo surgery, medical treatment is offered. These include painkillers, as well as hormonal medications. They are intended for symptom relief, and if the patient stops taking them, her symptoms will reappear and may even get worse.
The first-line preoperative medications are paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or diclofenac, which block the production of prostaglandins – hormone-like substances that trigger inflammation and pain. To be effective, they should be started at least 24 hours before a possible episode of pain (menstruation), when inflammatory substances have not yet built up. An additional benefit of taking this medication is a reduction in menstrual bleeding. It should be remembered that, as with any medication, these can have side effects, and prolonged use is not recommended.
There is currently a great deal of research into the mechanisms of pain in women with endometriosis. Studies show that if endometriosis is left untreated for a long time, pain that initially appears localised can become chronic, with changes in the central nervous system making it much more difficult to relieve.
Combined oral contraception basically relieves symptoms by suppressing the natural menstrual cycle and reducing the growth of endometriosis lesions. They have the advantage of being easy to use, with relatively few side effects. It is also important that combined contraception can be used in the long term.
However, it should be remembered that this approach is symptomatic and does not cure endometriosis. If use is discontinued, symptoms will reappear. Importantly, several studies have shown that some women with endometriosis (around 20%) also progress on combination contraception and are resistant to this treatment. This may be explained by the fact that endometriosis lesions generate their own hormonal environment for growth, making them less dependent on external conditions.
The use of these medications should be preferred in cases where the effective excision of the lesions has been performed and pregnancy is not currently planned, as they have been shown to reduce the risk of recurrence of endometriosis.
Like combined oral contraceptives, they reduce the symptoms of endometriosis by inhibiting the growth of endometrial lesions. This group also includes the medication dienogest, which is mentioned as a medication specifically for the treatment of endometriosis. From experience, it has a similar effect to combined contraception, and symptoms return after discontinuation.
Hormonal IUDs can also have a very good effect in adenomyosis, successfully reducing both pain and menstrual bleeding.
Medicines that cause menopause-like symptoms and are very effective in relieving pain. These medications are based on blocking the natural hormonal cycle of menstruation, which stops the growth of the lesions. Their biggest disadvantage is the side effects they cause and the fact that the long-term use of these medications (maximum 1 year with add-back therapy) is not recommended, as they reduce bone density. We sometimes prescribe this medication before surgery for deep endometriosis, as well as after surgery to reduce the risk of recurrence of symptoms and, as indicated in various studies, to improve the chances of getting pregnant.
Laparoscopy remains the only method that can accurately diagnose endometriosis and confirm it through the histological examination of tissue under a microscope. Laparoscopy is the standard surgical method for endometriosis today, as it provides excellent visualisation and reduces the risk of complications. Laparoscopic treatment ranges from small lesions to large lesions of deep endometriosis, which may require the excision of bowel, bladder, and other lesions.
The outcome of the surgery depends on the specialist’s experience in treating the condition. Not every doctor who performs laparoscopic surgery is an expert in endometriosis surgery, which is regarded as one of the most complex procedures in gynaecology today. From our experience, it’s hard to know exactly how long endometriosis surgery will take, since additional lesions are often found during the operation that don’t show up on ultrasound or MRI. To be effective, we believe that all lesions of endometriosis should be excised, as is done in leading centres around the world. Several studies have shown that the simple cauterisation (coagulation) of such lesions does not have the desired effect and should not be accepted as a treatment today.
For example, in the case of an endometriotic cyst, it is very often stuck to the pelvic wall. As the mechanism of endometrioma formation is different from that of cysts of other origins (endometriomas are formed by penetration of the ovarian capsule from the outside in), simply removing the cyst is not sufficient. We believe that complete removal of the original pelvic lesion on the pelvic wall is very important to reduce the risk of recurrence and avoid the need for repeated surgery. The safe excision of such lesions requires detailed knowledge of pelvic anatomy, as the surgery involves carefully separating tissues near structures such as the ureters and blood vessels – steps that are not typically a part of routine gynaecological surgery. Perhaps, for this reason, doctors sometimes limit themselves to removing the cyst and leave the technically difficult-to-remove lesions, believing that they can be treated with medication.
As the full significance of these lesions is unclear, and it is thought that they will not necessarily develop into typical or other endometriosis, they do not require special surgical treatment. To prove the diagnosis of endometriosis, these lesions must be excised.
Cutting out all these lesions is necessary to reduce pain and improve a patient’s chances of becoming pregnant. Depending on the location, such surgery can be technically demanding, requiring careful dissection around the ureters, blood vessels, and nerves to safely excise the lesion. As mentioned above, simply coagulating (cauterising) such lesions is not sufficient to treat them. Such lesions are best excised laparoscopically.
Several studies have shown that the most effective method is the complete removal of the cyst. The size of an endometriotic cyst (endometrioma) is not decisive – laparoscopy remains the primary treatment method, and laparotomy is no longer considered an option for endometriosis. The method of cyst removal is critical, as overly aggressive excision can damage healthy ovarian tissue and reduce fertility. Simply puncturing the cyst and cauterising the capsule is not desirable. Also, as mentioned above, removing the cyst is not sufficient. For the treatment to be complete, all lesions must be excised.
The most complex of endometriosis surgeries, it requires careful preparation and planning. In such cases, surgery often requires collaboration with a general surgeon and a urologist, as part of the bowel may need to be removed or the ureters and bladder may be affected. The aim of the surgery is to remove all the lesions of endometriosis. Deep endometriosis lesions can also be found on the diaphragm, so thoracic surgeons are sometimes needed for complete treatment. As with all types of endometriosis, deep lesions are treated using a laparoscopy.
| Type of endometriosis/treatment | The effect of surgery on pain | The effect of surgery on infertility | Risk of recurrence |
| Superficial – biopsy | Pain-free | No effect known | Rare |
| Typical – excision | Pain reduction for 50% of patients | Improves the outcomes of both spontaneous pregnancy and assisted fertilisation | About 20% in 10 years |
| Cystic – excision | Pain reduction for up to 90% of patients | Improves the outcomes of both spontaneous pregnancy and assisted fertilisation | Up to 5% in the case of effective surgery |
| Deep – excision | Reduction in 85% of cases | Improves the outcomes of both spontaneous pregnancy and assisted fertilisation | Up to 1% |
We believe that endometriosis is a surgically treatable condition, and surgery can have a very good effect if performed effectively.
There is often talk of treatment centres for endometriosis, but none currently exist in Latvia. If we take the United Kingdom as an example, Vītola klīnika meets the requirements of such a centre. More important than the centre, however, is a specialist who can provide honest and professional endometriosis treatment.
At Vītola klinika our specialists continuously update their knowledge by attending congresses and training worldwide, ensuring that women receive care aligned with the latest advances in endometriosis treatment. Dr Jurģis Vītols recently completed an internship at French Surgical Centre, whose leading specialists are among the pioneers in the world when it comes to the surgical treatment of deep endometriosis.
Incomplete surgical treatment occurs when not all the endometriosis lesions are excised, and the patient is not promptly referred to a specialist experienced in comprehensive endometriosis surgery
Symptoms caused by endometriosis can be similar to various other conditions (e.g., irritable bowel syndrome)
As the pain has been present since the onset of menstruation, it is perceived as normal
Long-term medical treatment is often used and may help at first – but unfortunately, endometriosis can sometimes continue to progress, even while taking hormonal medication
It is generally believed that endometriosis can always be diagnosed by gynaecological ultrasound or magnetic resonance imaging (the only 100% sure method is a diagnostic laparoscopy by an experienced specialist)
Endometriosis is diagnosed, but it is believed that it is impossible to operate on such a complex case in Latvia, so surgical treatment is postponed (the only gynaecological surgery that is not performed in Latvia is uterus transplantation)