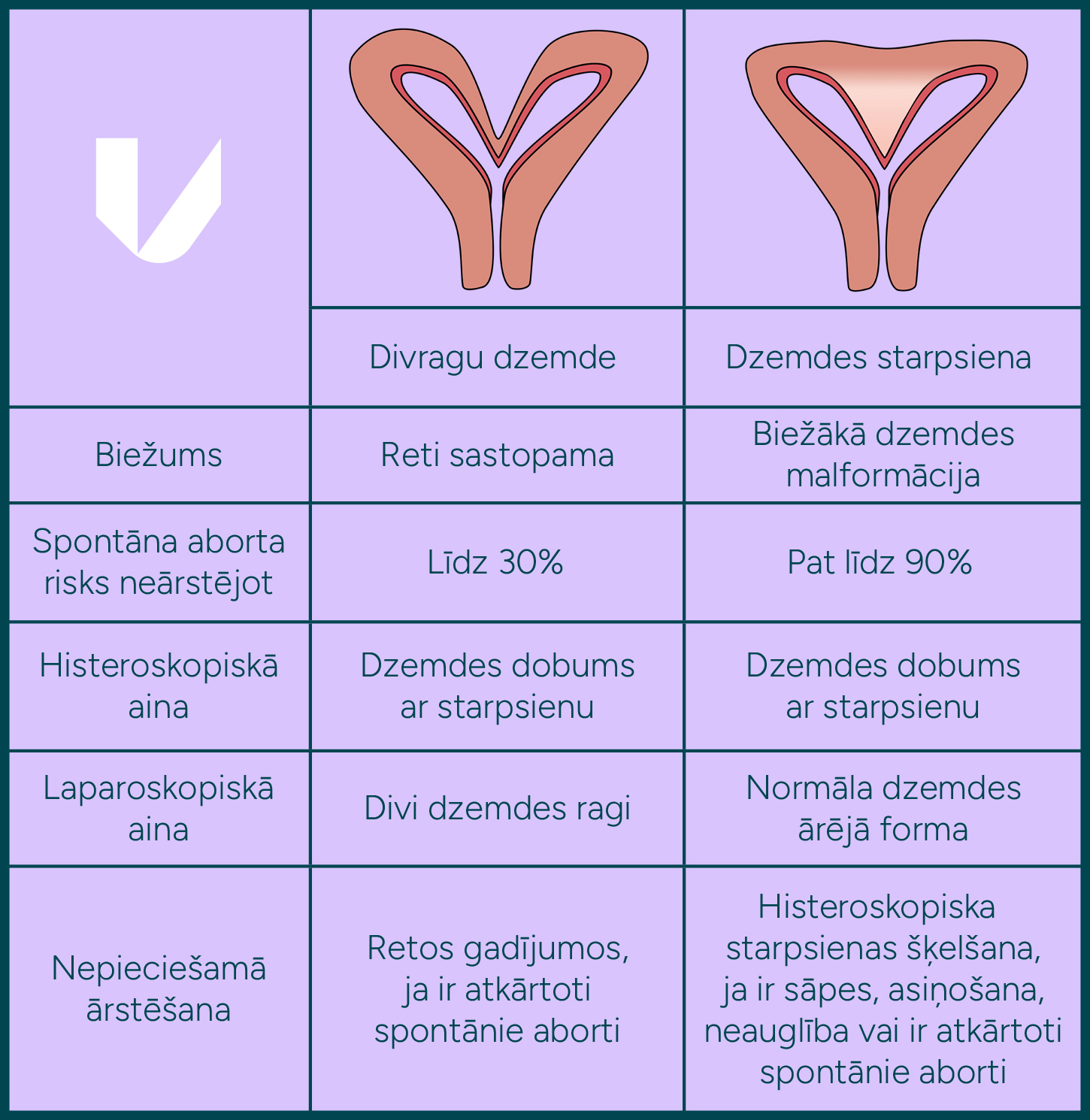
In daily practice, clinicians may occasionally encounter patients with changes in the uterine shape, detectable by ultrasound. Often, these women have painful periods, prolonged spotting, repeated miscarriages or infertility issues. When asked if the doctor has mentioned anything about the different shape of the uterus, the most common answer is that yes, they have a bicornuate uterus. Often, the real diagnosis is the presence of a uterine septum, and there is a significant difference. This distinction is particularly important in women presenting with pain, recurrent miscarriage, or infertility, since those with a septate uterus have been shown to have a higher risk of miscarriage and reduced fertility compared to women who have a bicornuate or normally shaped uterus. Nevertheless, this distinction is clinically significant, as a uterine septum can be treated relatively easily, with favourable outcomes when the procedure is performed by a gynaecologist experienced in hysteroscopy. In contrast, treatment of bicornuate uteri is most often unnecessary and surgical treatment, although possible, is difficult, and the results are not conclusive for the patient.
The exact incidence is unknown, as small uterine septa without clinical significance are relatively common but seldom cause symptoms. On the other hand, the more pronounced the uterine septum, the more likely it is to cause symptoms. It is thought to be between 1 and 15 cases per 1000 women. It is important to note that a uterine septum is the most common anomaly of uterine shape and occurs far more frequently than other malformations, such as a bicornuate uterus.
It should be remembered that a septum may not cause any symptoms and may be an incidental finding during an examination. However, some women with a uterine septum may present with severe dysmenorrhea, prolonged postmenstrual spotting, infertility, and recurrent early pregnancy loss. Although no studies have conclusively demonstrated that a uterine septum causes infertility, evidence suggests that surgical correction improves the likelihood of conception and reduces the risk of miscarriage.
For women with a septum who become pregnant, it can cause foetal malposition and premature birth
The reproductive organs develop during foetal life, while the foetus is still in the uterus. They are fully formed around the 20th week of pregnancy. The uterus develops from two Müllerian ducts, which fuse and differentiate to form the uterus, cervix, and upper third of the vagina. If this fusion process is disrupted, various uterine anomalies may occur, with the most common being a septate uterus. Less common anomalies include two uteri (characterised by two uterine cavities and two cervices) and a bicornuate uterus.
“In cases where the Müllerian ducts fail to fuse and the female genital tract does not develop, resulting in vaginal and uterine aplasia (Mayer–Rokitansky–Küster–Hauser syndrome), laparoscopic creation of a neovagina using the patient’s own tissue can be offered.
One of the less frequently described uterine anomalies, often associated with a small septum, is the T-shaped cavity, characterised by reduced uterine volume. This situation can also lead to infertility. Women with T-cavities usually have low-volume menstrual periods, although an ultrasound may give the impression of uterine wall adenomyosis.

If a uterine septum is suspected, a gynaecological ultrasound is recommended, as it can demonstrate both the shape of the uterine cavity and the external contour of the uterus. Gynaecological palpation (manual examination) can also help to understand whether there is one or two uterine bodies. It is very likely that a simple gynaecological ultrasound will suffice. If the external uterine contour is unclear, 3D sonography or an MRI may be performed, whereas hysterosalpingography or hysterosonography can be used to assess the configuration of the uterine cavity. Assessment of both the external and internal uterine morphology is essential in patients with recurrent miscarriage and infertility, unless another cause has been identified.
In the past, open surgery with a uterine incision was required to resect the septum. Today, with the advent of minimally invasive techniques such as hysteroscopy, these historical methods are no longer used. In scientific terms, the division and correction of a uterine septum is referred to as hysteroscopic metroplasty.
Hysteroscopy is an endoscopic surgical technique in which a hysteroscope – a slender instrument with a camera and light source – is introduced into the uterine cavity via the vagina and cervix. Small-diameter hysteroscopes (<5 mm) are now available and are particularly valuable in women who have not given birth, as this equipment can be used without cervical dilatation, thereby avoiding unnecessary trauma and reducing the risk of preterm birth. However, the choice of instruments depends on the length and width of the septum. After such surgery, the patient can return home in the evening of the same day. Depending on the thickness, width and length of the septum, adjuvant measures such as anti-adhesion gel, an intrauterine device, or other methods may be applied after surgery to reduce the risk of intrauterine adhesions.
As with a septum, a T-shaped uterine cavity can be treated hysteroscopically, with resection of the small septum and incision of the lateral uterine walls until a normal uterine shape and volume are restored.
Studies have demonstrated that hysteroscopic septal resection significantly reduces pain when present.
For patients who have difficulty becoming pregnant or have had repeated miscarriages, hysteroscopic resection or excision of the septum should be recommended. Research indicates that hysteroscopic septal resection improves the likelihood of pregnancy.
In cases where a septum is detected but pregnancy is not planned and no miscarriages have occurred, it is important to assess the size of the septum to determine whether surgical intervention is warranted.
In cases of a small septum without associated pain or spotting, pregnancy can be planned, with resection reserved for situations where conception does not occur or recurrent pregnancy loss develops. With a large septum, especially if there is pain and spotting after menstruation, we believe that the resection of the septum is preferable. However, each case is unique and requires specialist advice to make the best decision for the patient.
We consider that in cases where assisted reproduction is planned for other causes of infertility, hysteroscopic septum resection is recommended to improve the likelihood of pregnancy.
The biggest and most serious risk of such hysteroscopic surgery is the perforation of the uterus. To minimise its risk, it is important to differentiate the septal tissue from normal uterine wall tissue. The resection of the septum can be performed under sonographic control or under laparoscopic control to check the external shape of the uterus. In the event of uterine perforation, immediate laparoscopic surgery is required to assess the integrity of the abdominal organs and repair the uterine defect.
Another risk is the formation of adhesions, which, as mentioned above, can be prevented by various means. Other risks are relatively rare when a hysteroscopy is performed by an experienced specialist.
The inner wall of the uterus requires approximately eight weeks to heal, so it is considered safe to resume pregnancy planning two months after surgery.
CALL US:
+371 26 412 412Consultation with an experienced doctor is the first step towards taking care of your health and well-being.
AIZPILDIET PIETEIKUMA FORMU: