Endometrial polyps are growths arising from the lining of the uterine cavity and represent a common pathology in both women of reproductive age and those at menopause. It is one of the most common causes of heavy menstrual bleeding.
If you have already been diagnosed with a uterine polyp, at Vītola klīnika you can schedule its removal right away – without a prior consultation. The procedure is quick and gentle: the polyp can be removed within minutes, without mechanical dilation of the cervix, and for many patients – even without anesthesia. Minimal discomfort, fast recovery, and safety for the future.
When booking, please provide the following information:
• Ultrasound image: from Datamed or attach it by email to info@vitolaklinika.lv
or WhatsApp +371 26 412 412
• Menstrual cycle information: bleeding days + total cycle length
• Health insurance: indicate the name of your insurance provider
After receiving your request, we will contact you to arrange the most suitable date for the procedure.
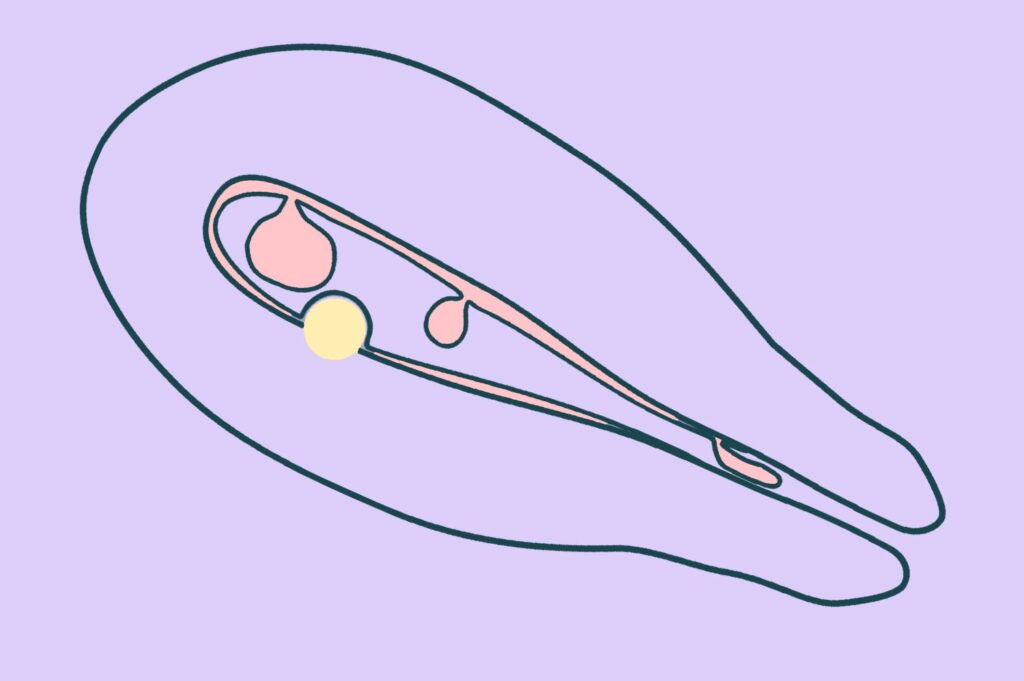
A polyp develops when there is localised overgrowth of the endometrium, the inner lining of the uterine cavity. Local gene mutations, hormonal changes, and the abnormal proliferation of individual cells contribute to the disruption of normal endometrial growth.
Increased menstrual bleeding is the most common symptom of polyps and occurs in ~70% of women with polyps.
Polyps rarely cause pain. This is possible in certain cases, most often when the polyp is very large.
There is no clear evidence that polyps cause infertility. However, if pregnancy does not occur and an endometrial polyp is identified, removal is recommended, as it may represent a contributing factor to infertility.
If a patient presents with abnormal uterine bleeding, one of the simplest diagnostic methods for detecting an endometrial polyp is a gynaecological ultrasound.
In unclear cases, the ultrasound should be repeated or a diagnostic hysteroscopy performed, which can also serve as an immediate treatment method.
If a polyp is located in the cervix or attached by a long stalk, it can sometimes be detected during a gynaecological examination.
In some women, small endometrial polyps may spontaneously regress or shed over time. However, if it is larger than 1 cm, the chance of the polyp disappearing without treatment is minimal.
Most polyps are made of benign cells, especially in younger women. However, in one out of 20 cases, malignant changes are found. It remains unclear whether a benign endometrial polyp can transform into a malignant lesion; however, the risk is higher in women receiving tamoxifen therapy for breast cancer. Malignant changes are more likely in patients with large polyps or pronounced bleeding symptoms.
If a woman has symptoms, the polyp should be removed, regardless of age.
It is also recommended to remove polyps if they are large (>1 cm), if there are more than one or if the patient has unexplained infertility.
If the woman has no symptoms, removal of the polyp should definitely be performed in patients at increased risk of endometrial cancer:
The most advanced and appropriate method for treating an endometrial polyp is hysteroscopic removal. Hysteroscopy is a minimally invasive surgical technique in which a polyp or other abnormal tissue is removed under direct visual guidance using a specialised instrument called a hysteroscope. This method has largely replaced uterine curettage (“uterine cleaning”), which is a blind procedure and is strongly discouraged in young women who wish to preserve fertility. Depending on its size, a polyp may be removed with a diagnostic hysteroscope (for small polyps) or with a resectoscope (for larger polyps). Even though dilation of the cervix is not necessary for a diagnostic hysteroscopy, it is required for a hysteroresectoscopy. Cervical dilatation can cause cervical trauma, which can affect future pregnancies. Similarly, a hysteroresectoscopy uses electricity, which, if not used accurately, can cause deeper damage to the inner layer of the uterus.
Today, JV Clinic offers an innovative technique – the IBS (Intrauterine Bigatti Shaver) system – based on mechanical energy, which enables the precise and rapid removal of polyps while minimising damage to the surrounding tissue. Such a system is only available in Latvia at the Vītola klīnika and the Embrions Clinic. Importantly, this method does not require cervical dilation and, in some cases, can even be performed without anaesthesia.
CALL US:
+371 26 412 412Consultation with an experienced doctor is the first step towards taking care of your health and well-being.
AIZPILDIET PIETEIKUMA FORMU: