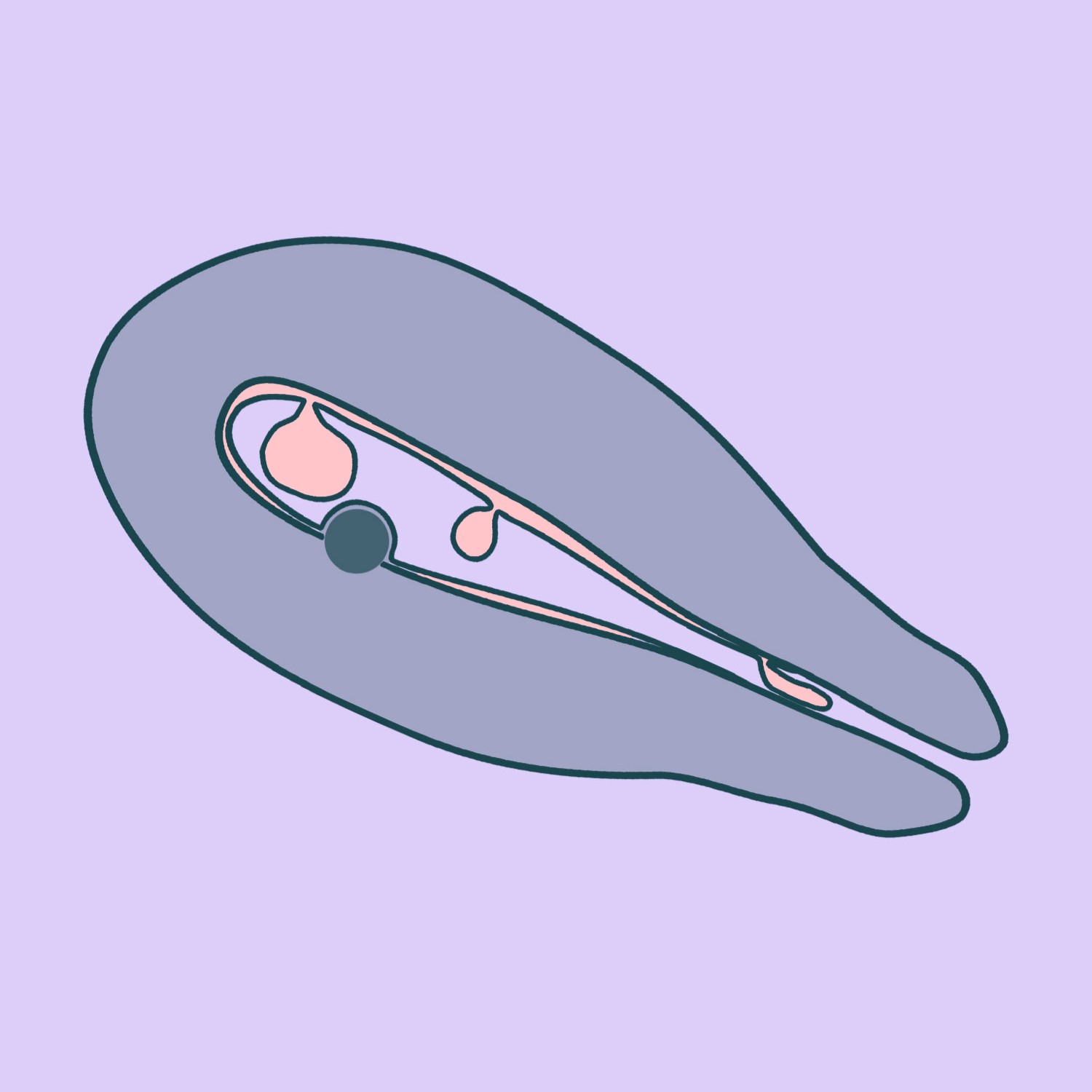
Hysteroscopy is a minimally invasive surgical procedure that enables the removal of uterine abnormalities – such as polyps, submucosal fibroids, or other abnormal tissue – from the uterine cavity under direct visual guidance. Hysteroscopy also makes it possible to remove displaced or “missing” intrauterine devices (IUDs), correct abnormalities in the shape of the uterine cavity, resect adhesions, and perform other intrauterine procedures. The procedure is most commonly performed under short-term intravenous anaesthesia, although in some cases, it can be carried out without anaesthesia. We use small-diameter hysteroscopes, which eliminate the need for cervical dilation – an important advantage, particularly for women who have not given birth. The excised pathological tissue is sent for histological examination after surgery.
Preparing for the Test and Choosing the Right Time
Required Tests and Referrals for Patients Undergoing Hysteroscopic Polyp Resection with Short-Term Intravenous Anaesthesia
Required Tests and Referrals for Patients Undergoing Hysteroscopic Polyp Resection without Anaesthesia
In our clinic, hysteroscopic polyp resection is performed using the “no-touch” technique, in which a small-diameter hysteroscope is introduced through the vagina and into the uterus without the need for additional instruments, thereby avoiding cervical dilation with dilators. The procedure begins with a vaginoscopy, performed without the use of speculums or tenacula, during which the hysteroscope is advanced to the cervix under direct visual guidance. Using warm and sterile saline, gentle cervical dilatation is performed, which allows penetration of the uterine cavity. The shape of the cavity, its size, the fallopian tubes, and the endometrium are assessed. During surgery, the polyp is removed either mechanically – using scissors or a specialised IBS instrument – or with laser energy. The excised material is sent for histological examination.
You can go home a few hours after the surgery.
After a hysteroscopy, it is recommended to rest for 24–48 hours. You can resume exercising and other more intensive activities 2–3 days after surgery. Abstain from intercourse, swimming, taking a bath and using a sauna for 2 weeks. Further recommendations are made before the patient is discharged home.
CALL US:
+371 26 412 412Consultation with an experienced doctor is the first step towards taking care of your health and well-being.
AIZPILDIET PIETEIKUMA FORMU: